Treatment & Disease Management of Dermatomyositis
Goals of therapy
Dermatomyositis, similar to polymyositis10, requires a multidisciplinary approach involving rheumatologists, dermatologists, neurologists, pulmonologists, pathologists, physiotherapists and occupational and speech therapists.1-3,11
Therapy often involves a combination of pharmacological and non-pharmacological (e.g. exercise) approaches to work towards the following goals.
| Goals of therapy | Impact on the patient1,3 |
|
Pharmacological treatment options for dermatomyositis
The goal of pharmacological treatments for dermatomyositis is to reduce inflammation, improve muscle strength and stabilise the disease.2
In absence of consensus guidelines for the treatment of idiopathic inflammatory myopathies, dermatomyositis patients are treated based on symptoms and disease severity.4
Immunosuppressive therapy is widely accepted as the mainstay of treatment for idiopathic inflammatory myopathies, with corticosteroids – commonly prednisone – widely used as first-line therapy.2,4
Other immunosuppressants and/or intravenous immunoglobulin (IVIg) treatment are commonly used as second- or third-line therapies to avoid the serious side effects of prolonged corticosteroid use.2,4
IVIg can be used in patients with active dermatomyositis treated with immunosuppressive drugs including corticosteroids, or with intolerance or contraindications to those drugs.4
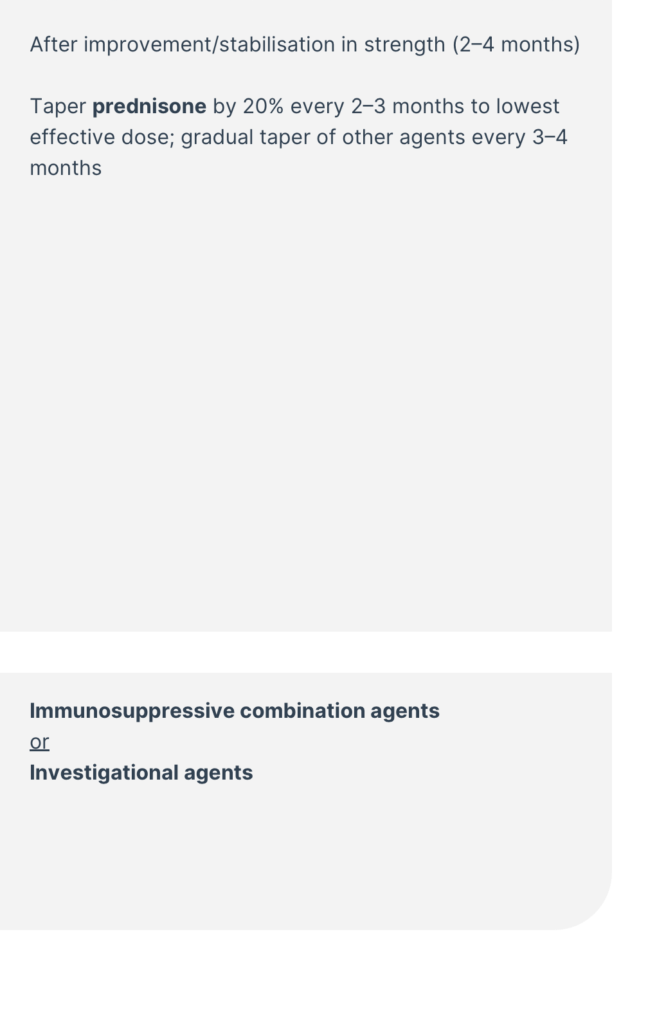
Suggested treatment algorithm for patients with immune-mediated myopathies4
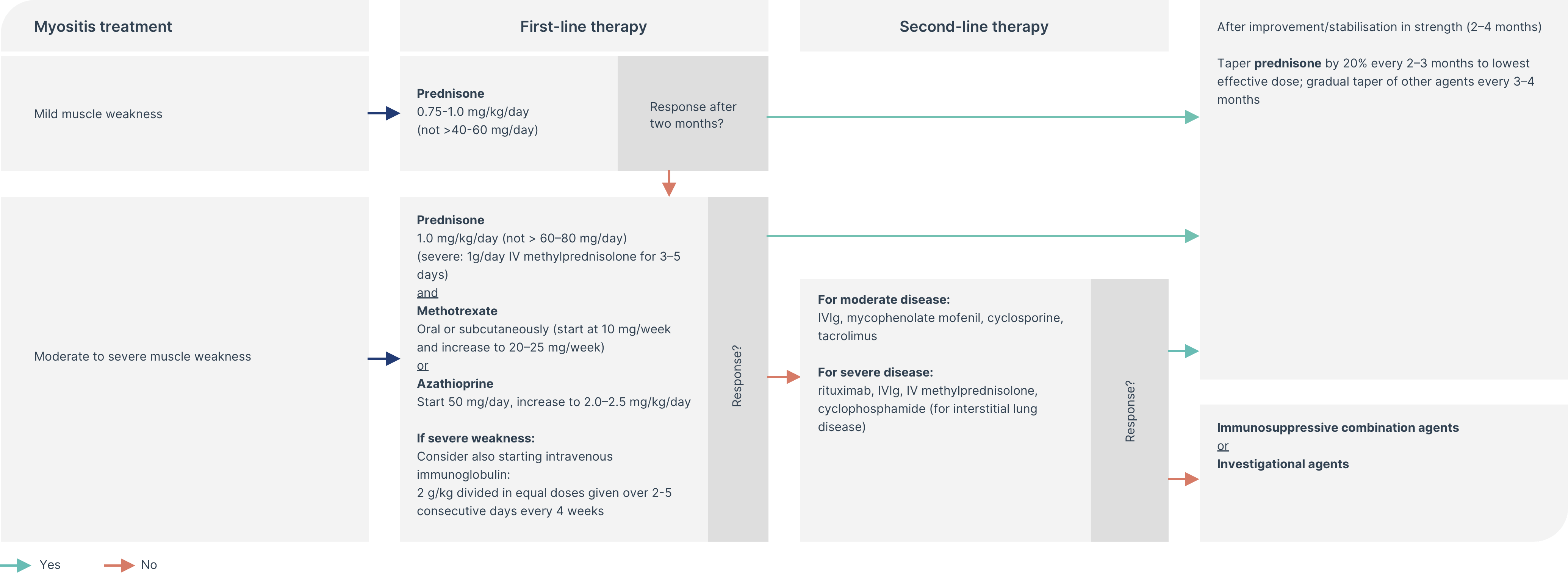
*Disclaimer: The treatments mentioned above are not necessarily approved in all countries for use in patients with dermatomyositis. All recommendations, including dosing regimens, are based on the opinions of the authors of the cited publications. Treating physicians should always refer to the relevant package insert in their country before prescribing a product.
The degree of muscle weakness (mild or moderate/severe) helps to guide the dose of prednisone.4
In cases of moderate/severe muscle weakness, immunosuppressive therapies are usually started in parallel with corticosteroids.4
In cases of severe muscle weakness, intravenous corticosteroids are indicated.2,4
Depending on treatment response, and whether weakness is persistent or if there is other organ involvement, therapy can be escalated or de-escalated.2
Properties of agents recommended as potential therapies in idiopathic inflammatory myopathies
| Category2,4 | Molecule2,4 | Posology4 | Effect | Side effects2 |
| Corticosteroids |
|
|
|
|
| Immunosuppressants |
|
| Immunosuppressive |
|
| Intravenous immunoglobulin |
|
| Immunomodulatory |
|
Properties of other therapies for idiopathic inflammatory myopathies
| Category2,4 | Molecule2,4 | Posology4 | Effect | Side effects2 |
| Immunosuppressants |
|
| Immunosuppressive |
|
| Calcineurin inhibitors |
|
|
| |
| Monoclonal antibody anti-CD20 | Rituximab | Initially 2x 1 g followed by 1x 1 g every 6 months |
|
|
Pharmacological treatment options for juvenile dermatomyositis
Evidence to support treatment options in children with dermatomyositis is still lacking, and there are no approved therapies.
Similarly to adults, the mainstay of therapy is use of corticosteroids in combination with immunosuppressive therapies.5
Adopting an early, aggressive treatment approach may prevent or stabilise organ damage and the associated disease complications such as calcinosis, the latter being associated with significant morbidity due to pain and infection risk.5
Non-pharmacological management options for dermatomyositis
| Approach | Benefits |
| Physiotherapy and occupational therapy1 |
|
| Physical training | |
| Maintenance of healthy bodyweight6 |
|
| Improvement of diet and nutrition9 |
|
| Avoidance of UV exposure1,6,8 (e.g. use of sunscreen and appropriate cover to limit sun exposure) |
|
| Mindfulness6 |
|
| Stopping smoking |
|
References
- Malik, A., Hayat, G., Kalia, J. S., & Guzman, M. A. (2016). Idiopathic Inflammatory Myopathies: Clinical Approach and Management. Frontiers in Neurology, 7. https://doi.org/10.3389/fneur.2016.00064
- Glaubitz, S., Zeng, R., & Schmidt, J. (2020). New insights into the treatment of myositis. Therapeutic Advances in Musculoskeletal Disease, 12, 1759720X1988649. https://doi.org/10.1177/1759720x19886494
- Dalakas, M. C., & Hohlfeld, R. (2003). Polymyositis and dermatomyositis. The Lancet, 362(9388), 971–982. https://doi.org/10.1016/s0140-6736(03)14368-1
- Goyal, N. A. (2019). Immune-Mediated Myopathies. CONTINUUM: Lifelong Learning in Neurology, 25(6), 1564–1585. https://doi.org/10.1212/con.0000000000000789
- Bellutti Enders, F., Bader-Meunier, B., Baildam, E., Constantin, T., Dolezalova, P., Feldman, B. M., Lahdenne, P., Magnusson, B., Nistala, K., Ozen, S., Pilkington, C., Ravelli, A., Russo, R., Uziel, Y., van Brussel, M., van der Net, J., Vastert, S., Wedderburn, L. R., Wulffraat, N., & McCann, L. J. (2016). Consensus-based recommendations for the management of juvenile dermatomyositis. Annals of the Rheumatic Diseases, 76(2), 329–340. https://doi.org/10.1136/annrheumdis-2016-209247
- John Hopkins Myositis Center. Living with dermatomyositis; https://www.hopkinsmyositis.org/educational-resources/dermatomyositis-lifestyle-options: Last accessed 19.07.2021;
- The Myositis Association. Diet and nutrition; https://www.myositis.org/about-myositis/treatment-disease-management/complementary-and-self-care-therapies/diet-and-nutrition/: Last accessed 18.10.2021;
- Oddis, C., & Aggarwal, R. (2018). Treatment in myositis. Nature Reviews Rheumatology. https://doi.org/10.1038/nrrheum.2018.42
- Lilleker, J. B., Vencovsky, J., Wang, G., Wedderburn, L. R., Diederichsen, L. P., Schmidt, J., Oakley, P., Benveniste, O., Danieli, M. G., Danko, K., Thuy, N. T. P., Vazquez-Del Mercado, M., Andersson, H., De Paepe, B., deBleecker, J. L., Maurer, B., McCann, L. J., Pipitone, N., McHugh, N., & Betteridge, Z. E. (2018). The EuroMyositis registry: an international collaborative tool to facilitate myositis research. Annals of the Rheumatic Diseases, 77(1), 30–39. https://doi.org/10.1136/annrheumdis-2017-211868
- M. King, W. and Kissel, J.T. (2013). Multidisciplinary Approach to the Management of Myopathies. CONTINUUM: Lifelong Learning in Neurology, 19, pp.1650–1673. doi:https://doi.org/10.1212/01.con.0000440664.34051.4d
- Kohsaka, H., Mimori, T., Kanda, T., Shimizu, J., Sunada, Y., Fujimoto, M., Kawaguchi, Y., Jinnin, M., Muro, Y., Ishihara, S., Tomimitsu, H., Ohta, A. and Sumida, T. (2018). Treatment consensus for management of polymyositis and dermatomyositis among rheumatologists, neurologists and dermatologists. The Journal of Dermatology, 46(1), pp.e1–e18. doi:https://doi.org/10.1111/1346-8138.14604
Science Hub
Sign up and connect to Science Hub to learn more about our recent ProDERM study and have access to symposia presentations, publications, posters and lectures.
